Dr. Jess Rushing is a Fellow of the National Institute of Infant and Child Medical Music Therapy and is currently the chair of the American Congress of Rehabilitation Medicine (ACRM) Arts and Neuroscience Networking Group. She has worked clinically with all ages, from premature infants to end-of-life, with considerable experience in medical, private practice, and mental health. Dr. Rushing’s research interests include music therapy in acute post-stroke care, music therapy supervision, and community engagement.
Dr. Jess Rushing is a Fellow of the National Institute of Infant and Child Medical Music Therapy and is currently the chair of the American Congress of Rehabilitation Medicine (ACRM) Arts and Neuroscience Networking Group. She has worked clinically with all ages, from premature infants to end-of-life, with considerable experience in medical, private practice, and mental health. Dr. Rushing’s research interests include music therapy in acute post-stroke care, music therapy supervision, and community engagement.
Book Collaboration
Dr. Jayne Standley invited Dr. Rushing to collaborate on the third edition of Evidence-Based Music Therapy for Premature Infants. The book was published by Silver Spring, MD: American Music Therapy Association, Inc., in 2023.
Dr. Standley is an internationally acclaimed researcher and has published extensively. A Robert O. Lawton Distinguished Professor at Florida State University, she directs the Music Therapy program, the National Institute for Infant and Child Medical Music Therapy, which awards the NICU-MT national certificate, and the Medical MT and Arts in Medicine Programs in partnership with Tallahassee Memorial HealthCare.
Dr. Rushing said, “As a bright-eyed freshman at FSU, I learned that Jayne Standley was perhaps the most accomplished and renowned medical researcher in the field of music therapy. She specifically, pioneered an evidence base for NICU music therapy practices.” Dr. Standley inspired Dr. Rushing’s career interest in NICU scholarship. Rushing said, “My first full-time employment was at Tallahassee Memorial Hospital, which was the location of much of her research. Throughout my academic journey, I was honored to learn from and work under Jayne in the NICU and on research projects.”
“My philosophy is to help students love doing research while learning the skills for same and to provide as many opportunities as possible within their interest areas to promote their success. This helps the student define their own research focus and furthers knowledge within the field of study,” said Dr. Standley.
Dr. Rushing contributed to the book by updating the literature and adding pieces relevant to health care as it has evolved since the last edition. “I wanted to make sure that music therapists would have the most up-to-date information possible to feel confident to walk into a NICU with a foundational understanding,” she said.
“Her meticulous scholarship and avid interest in this area made her a wonderful collaborator,” said Dr. Standley.
Book Summary
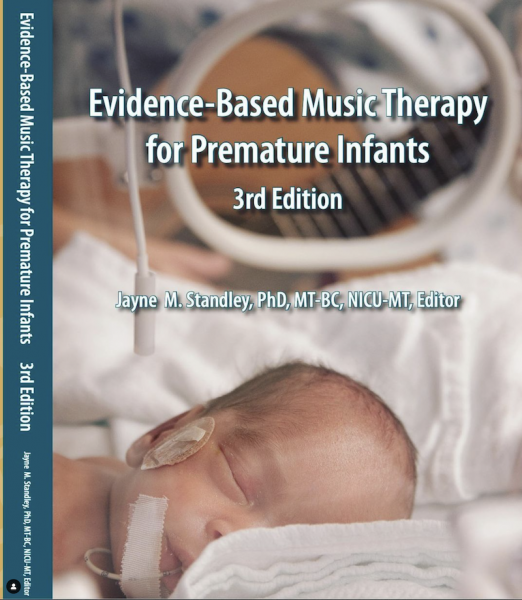 Evidence-Based Music Therapy for Premature Infants, Third Edition
Evidence-Based Music Therapy for Premature Infants, Third Edition
Over 30 years of research and clinical practice in music therapy with premature infants has been compiled into this text designed for Board Certified Music Therapists specializing in Neonatal Intensive Care clinical services, for NICU medical staff incorporating research-based music therapy into developmental care plans, and for parents of preemies desiring to improve their child’s quality of life. Contents include complications of premature births, typical medical/developmental assessments, NICU care procedures, infant growth and maturation goals desirable during the last trimester of neurological development, and clinical music therapy procedures to facilitate these goals. Edited by Jayne Standley, PhD, MT-BC, MT-NICU.
Rushing, J. & Standley, J. M. (2023). Medical care of the premature infant. In J. M. Standley (Eds), Evidence-based music therapy for premature infants (third edition) (pp. 22-31). Silver Spring, MD: American Music Therapy Association, Inc. Rushing is a regular presenter for the National Institute of Infant and Child Medical Music Therapy, where they certify music therapists who work in NICUs. “This chapter is the foundation for working in a NICU,” said Rushing.
Research and knowledge about the care of premature infants has greatly expanded since the first edition of the book, which was released 20 years ago. “Current research in music therapy demonstrates multiple benefits for neurologic development, feeding, bonding, and stress reduction of infants while reducing the length of their hospitalization in the NICU,” said Dr. Standley. “NICU-MT has expanded into perinatal services to reduce stress of pregnant women hospitalized to forestall premature labor. NICU-MT is also providing in -home services following discharge to help mothers promote developmental milestones of their still vulnerable infants born prematurely and at-risk for developmental delay.”
In two of Rushing’s courses at CSU – Introduction to Music Therapy and Medical Music Therapy Methods – there is regular discussion about what it means for an infant and family to receive care in a NICU. Rushing said, “We learn about what it means to receive care in the NICU, medically, environmentally, and from an interprofessional standpoint, in addition to the role of music therapy techniques. The information aids music therapists in knowing what to look for in medical chart reviews and how to understand what might be happening for an infant medically may impact their music therapy treatment.”
The NICU, which has its own culture, language, and workflow, can be an intimidating environment. Rushing hopes that the chapter helps music therapists feel confident and knowledgeable enough to assume their role as healthcare professionals in the NICU. Rushing said, “I hope that in reading the chapter and the rest of the book, music therapists can feel well positioned to play a valuable role in the growth and development of our smallest clients and their care partners.
Evidence-Based Music Therapy for Premature Infants, Third Edition: ISBN #978-1-884914-38-6, Publication date: 2023
Authors: Jayne M. Standley PhD, MT-BC, NICU-MT; Andrea Cevasco-Trotter PhD, MT-BC, NICU-MT; Cassi Crouse MM, MT-BC, NICU-MT; Darcy DeLoach PhD, MT-BC, NICU-MT, Judy Nguyen Engel MM, MT-BC, NICU-MT; Ellyn Hamm Evans PhD, MT-BC, NICU-MT; Abigail L. Foster MM, MT-BC, NICU-MT; Lori Gooding PhD, MT-BC, NICU-MT; Flor de Cielo Hernandez PhD, MT-BC, NICU-MT; Dawn Iwamasa PhD CCLS, MT-BC, NICU-MT; Ciele Knox MM, MT-BC, NICU-MT; Chris Millett MM, MT-BC, NICU-MT; Brianna Negrete MM, MT-BC, NICU-MT; Jennifer Jarred Peyton MM, MT-BC, NICU-MT; Emily Pivovarnik MM, MT-BC, NICU-MT; Amy Robertson PhD, MT-BC, NICU-MT; Jess Rushing PhD, MT-BC, NICU-MT; Lorna Segall PhD, MT-BC, NICU-MT; Hannah Sellers, MM, MT-BC, NICU-MT; Deborah Stevens, MM, MT-BC, NICU-MT; Valerie Williams, MM, MT-BC, NICU-MT; Natalie Wlodarczyk, MT-BC, NICU-MT; Olivia Swedberg Yinger PhD, MT-BC, NICU-MT.